By intellircm 12th Nov 2022 Blog
Claims denials are avoidable!
In fact, 90% of these denials are completely avoidable, and with more effective denial claims management, you can still receive payments for services rendered.
If left unpaid, claims denials pose a significant risk to the financial wellness of your practice. We recommend outsourcing medical claims denial management to experienced claims specialists.
That said, the best way to manage claims denials is by avoiding them in the first place. We recommend these steps to reduce the claims denial rates at your medical practice.
7 Steps to Reduce Claims Denial Rates
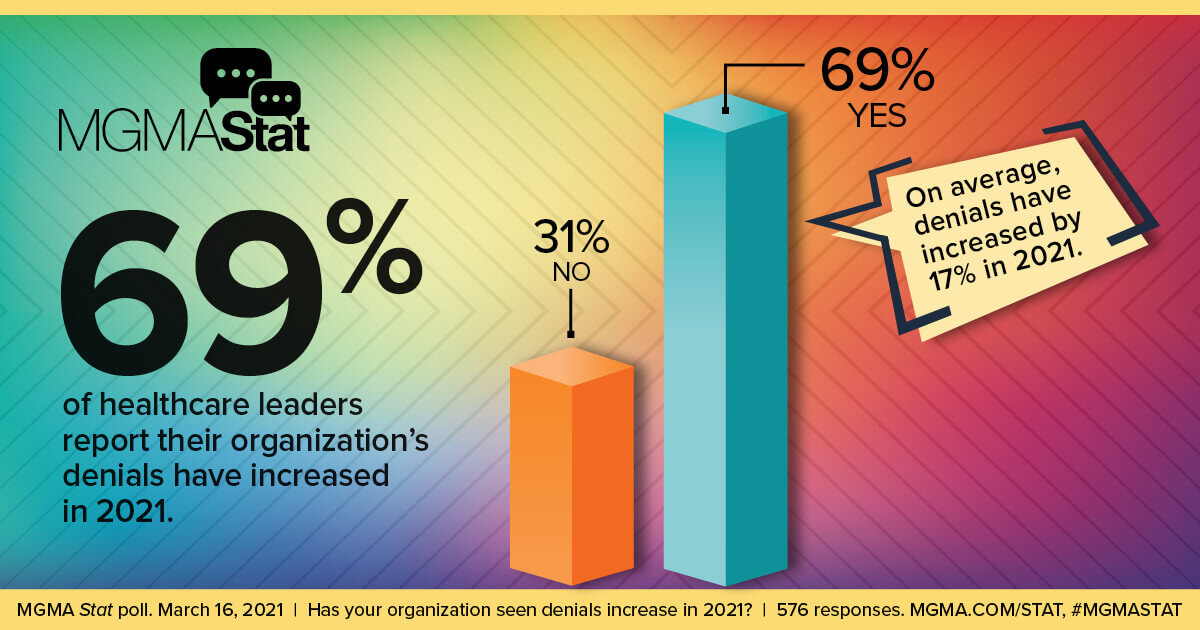
Medical claims denials are on the rise. There were more claims denials last year than in previous years, many of which are due to simple reasons like Eligibility & Benefits Verifications not being completed or not done properly. Perhaps action wasn’t taken on EVBV, missing or incorrect codes, or patient identifiers. Spelling errors can even cause insurance providers to deny claims.
Here are our seven tips for reducing claim denials.
1. Verify Patient Information Up Front
Many medical offices and hospitals are busy and understaffed. Unfortunately, that means there are times when patient information is incomplete, and no one verifies that data with the patient before they leave the facility or AR files the claim for payment.
In a study published by the American Medical Association (AMA), 94% of doctors claim prior authorization delays adequate patient care, and nearly half go on to admit it has caused claims denials.
That's why we recommend training your administrative staff to collect vital information immediately upon admission. Software tools can help ensure that "every box gets checked" throughout the registration and enrollment process. It saves time and potential entry errors over manual processes.
2. Remind Patients of Their Responsibility
One issue with claims denials might be the failure to communicate who is (and isn't) responsible for the payment of certain services. You may place a sign at the front desk reminding patients that they are responsible for charges their insurance doesn’t cover.
We suggest including a standardized form for your patients to fill out explaining their financial obligations once your office submits claims to all parties for payment. You should also post this information on your website, newsletters, and emails.
3. Enhanced Claims Management Training
During onboarding, make sure new staff receive training on your practice’s systems, including the claims filing process, documentation collection, and steps to check data accuracy. Implement best practices and offer retraining or internal certification processes to ensure competence.
4. Submit Claims Sooner
According to claims specialists, insurers deny claims because of issues associated with "timely filing." Any medical team can easily correct this by filing claims sooner.
Batch claims and submits them according to a pre-set schedule. Identify delays and address oversights. Make sure not to overwork your staff because this can lead to errors like claims processing delays.
5. Hire Consultants to Perform Audits
Never go at claims processing alone. You are a medical provider. You specialize in patient care. Talk to a claims processing and denial professional to help you set up automation and digital processes to replace manual tasks.
That will help reduce errors. It will also ensure your team doesn't omit vital information, wait to file a claim or do anything else that could lead to the denial of a claim.
6. Upgrade Your Computer Systems
Another reason for claims denials is that medical practices don't update their computer systems, leading to inefficiencies and errors. Modern computer systems help your staff be more productive and less likely to make claims errors.
7. Implement Software for Denial Management
Along with upgraded computer systems, your medical practice will need software for managing medical billing and coding. Make sure the software solution handles denied claims and everything else your practice needs from a revenue cycle management platform.
Prioritizing Claims Denials Reduction
Fewer claims denials offer your budget some flexibility, allowing you to devote additional resources to providing the best possible patient care. At IntelliRCM, we deliver a revenue cycle management solution that can handle claims denials so that you don't have to worry about invoices being left unpaid.
Time to upgrade your revenue cycle management to avoid claims denial? Contact one of our friendly professionals to learn more.





