By intellircm 20th Jun 2023 Blog
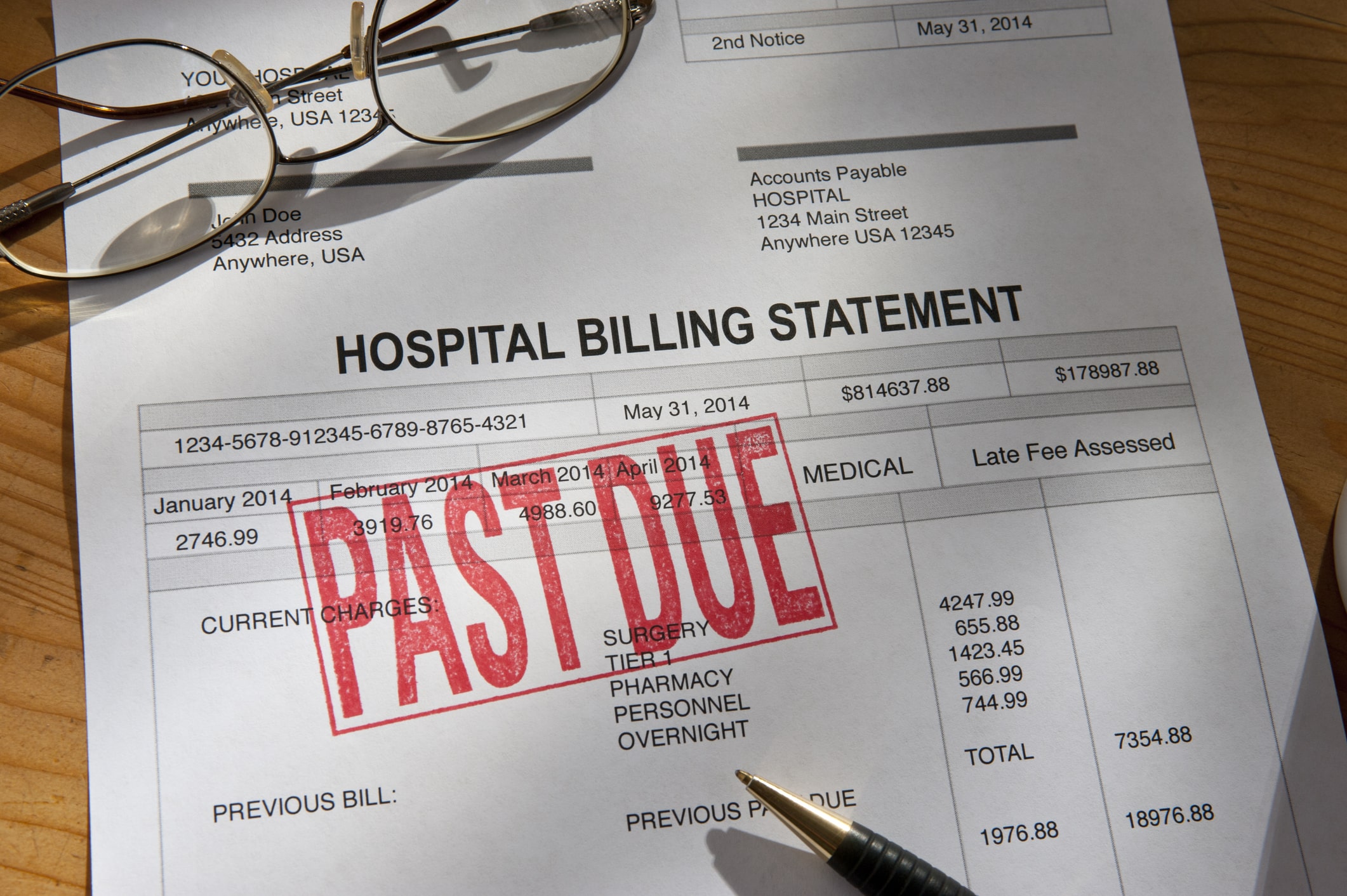
Widespread concerns about the cost of healthcare drove the U.S. government to enact the No Surprise Act. While the law helps make healthcare more affordable and accessible, it poses a significant challenge to healthcare providers. It introduced new accounting requirements to a sector buckling under existing regulations.
Failure to meet these dynamic requirements can leave health practices struggling financially. It leads to increased claim denials and claim disputes. If your health practice is facing financial headwinds, IntelliRCM can help. We offer revenue cycle management services to ensure healthcare practices are paid in full and on time.
What Is the No Surprise Act?
The No Surprise Act is a federal law that protects patients from unexpected medical bills whenever they seek healthcare outside their insurer's network. The law requires healthcare services and insurers to provide patients with simple, clear, and understandable information about out-of-network care coverage and costs.
It also provides a framework for resolving payment disputes that may arise between care providers and insurance companies.
Under the No Surprise Act, healthcare providers shouldn't hike prices for patients who seek medical services outside their insurance network. Previously, health practices charged higher to cover the additional cost of collecting payments.
The law also prohibits balance billing. Care providers can't bill patients for any pending balance after the insurer pays their share of the bill. While laudable, the No Surprise Act requires healthcare practices to rethink and streamline their accounting and billing systems. It creates an additional hurdle that could delay payments and cause them to extend beyond the claim timeframe.
The Implication of the No Surprise Act on Medical Billing
The No Surprise Act has a far-reaching impact on medical accounting and billing systems and processes. These implications include:
A Need for an Electronic Medical Billing System
Switching to electronic billing simplifies compliance. Healthcare providers can seamlessly implement the new coding and billing protocols. The recent changes ensure patient charges never exceed the legally established qualifying payment amount. More importantly, they can automate the process of issuing a written rights notice. Federal law requires healthcare facilities to give patients hard copies of the notice of their rights under the law. The notice covers:
- The right to receive out-of-network care
- The potential costs of out-of-network care
- Protection against balance billing
Besides generating notices on-demand, care providers must ensure patients have ready access to billing information and understand their rights under the new law.
A Need to Renegotiate Contracts
The No Surprise Act requires insurance companies to pay a qualifying payment amount for out-of-network care. The amount is based on the median in-network for similar services in the geographic area. Establishing the qualifying amounts is a complex process that accounts for multiple factors.
A provider's accounting and billing system must be flexible and dynamic to accommodate new changes. That requires new protocols to capture out-of-network care and then bill the relevant insurer. It may also necessitate new accounting practices to track the costs and capture all the necessary details.
Only then can a healthcare provider engage meaningfully with insurers and protect their bottom line. A dynamic medical billing and accounting system enables them to protect their profit margins while remaining compliant with the law.
A Need to Develop New Billing Dispute Processes
No Surprise Act requires providers and insurance firms to enact new protocols when resolving out-of-network care billing disputes. The law allows a 30-day negotiation window for the providers and insurers to resolve the dispute amicably. The dispute becomes subject to a binding arbitration process if they can't reach an agreement.
Complying with these requirements calls for innovative billing and accounting solutions. They need a system capable of tracking and reporting out-of-network care disputes.
Electronic medical billing systems ensure providers have the necessary documents to support their claims during dispute resolution proceedings. That may also require them to develop new reporting and reporting processes that comply with the law.
Protect Your Bottom Line and Improve Customer Experience
Switching to an electronic medical billing system protects your bottom line while ensuring your practice complies with the No Surprise Act. Working with an expert revenue cycle management service can accelerate compliance and reduce errors.
At IntelliRCM, we deliver custom revenue cycle management services to healthcare providers. You can count on our vast experience and expertise to equip you with the tools and services to grow your health practice.
Need help streamlining your out-of-network billing process? Book a free consultation today!





